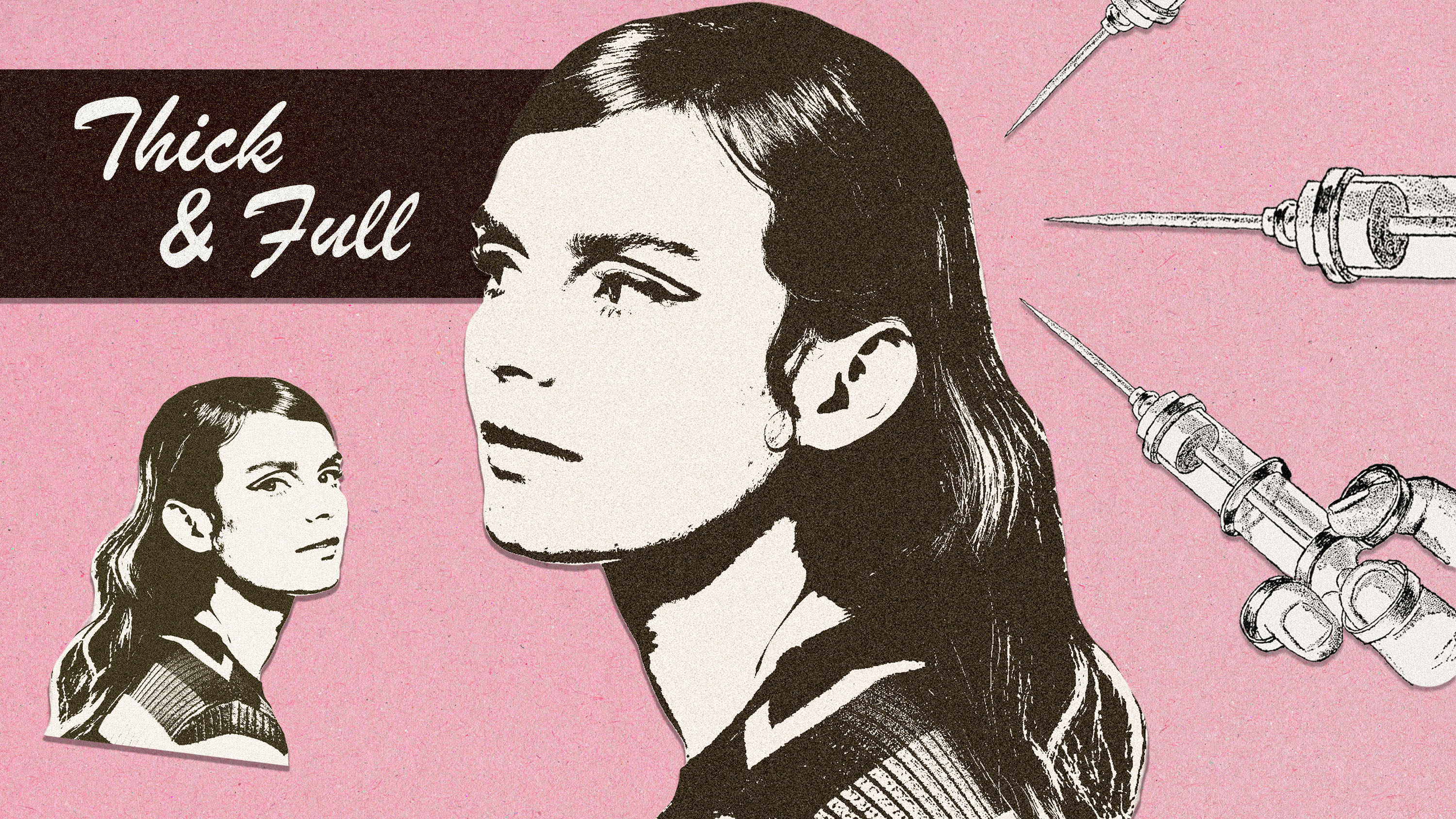
I Get My Own Blood Injected Into My Scalp
I have premature androgenic alopecia and do it in the name of hair growth.

It may sound silly, but having great (not good, great) hair has been a trademark of my personality since I came out of the womb. Literally—I was born with a full head of hair. As I grew up, I became hyper-fixated on having the best hair in the room at all times. It could be 95 degrees and humid at sleepaway camp, and I would force myself to get up two hours early to wash, blow dry, straighten, and curl my whole head. Since middle school, I’ve refused to leave the house with a hair out of place or, god forbid, in a ponytail.
I’d be lying if I didn’t admit that having a good hair day, every damn day, didn’t become synonymous with my identity somewhere along the way. I have other things going for me, don’t get me wrong, but my perfectly manicured, evenly parted, wildly healthy hair has long been my security blanket.
Cut summer 2021. My hair was, well, not my hair. My texture went from thick and full to thin, scraggly, and borderline see-through. I’ve been a hair-to-mid-boob girl my whole life, but out of left field, it became armpit length. I didn’t get a haircut. I chalked it up to stress? Maybe COVID-19 hair loss? It just continued to get worse. And worse. And worse. I hyper-fixated on old photos trying to discern if it was actual hair loss or if I was simply delusional.
A few months later, people started commenting. Did you get a haircut? Did you do something different? You look different. “Different” was the key word and it soon became my trigger. I’m not going to stand here and say I have the worst hair loss to date. Absolutely not. I have it pretty lucky all things considered. But, my hair was, without a doubt, different. It didn’t matter how many volumizing shampoos and thickening mousses I threw at myself. My security blanket was gone and I permanently felt like the Hot Mess Express. I avoided mirrors and started wearing my hair up in a bun for the first time in my entire life. And I developed a pit in my stomach every time a hair stylist gave me innocent styling tips for “thin” hair.
After a few months of dread, I went to my dermatologist, Dr. Sapna Palep. It was June 14, 2022. I told her my saga, she asked for my medical history (I have PCOS, for the record), and within no more than two minutes she looked me in the eyes and said, “You have androgenic alopecia.” My stomach jumped into my throat and panic set in. How? How at the ripe old age of 26 did I have alopecia? What did that mean? What were my options? Was I going bald? I was firing questions in her direction at the speed of light.
I knew this wasn’t a death sentence, the end of the world, or the worst diagnosis in the world. Relatively speaking, I’m damn lucky. But I have an emotional attachment to my hair and the thought of losing it threw me for a freakin’ loop.
“All women will go through androgenic alopecia at some point, but most women will go through it more rapidly when they’re post-menopausal,” Dr. Palep told me. Reason being, when you’re postmenopausal, your estrogen plummets and testosterone takes over. One side effect of this newfound imbalance is that hair follicles “fall asleep,” so to say.
Get exclusive access to fashion and beauty trends, hot-off-the-press celebrity news, and more.
I have a good couple decades until I’m postmenopausal, so why was this happening? The answer was hormones. I have polycystic ovary syndrome, which changes the game. Following bloodwork, it was determined that I have elevated luteinizing hormone, which among other things can increase my testosterone. “There are many different kinds of PCOS, but your specific PCOS puts you in premature androgenic alopecia,” Dr. Palep tells me. “Your PCOS paired with the fact that your hair is not growing as long and is gradually thinning is proof that the hormones are trying to miniaturize your hair follicle.”
Information is power. So after going over my options, and regrettably going down one too many Reddit rabbit holes, I decided to take a two-prong treatment approach. Dr. Palep prescribed me Spironolactone, an androgen suppressant that's thought to help with hair loss. It’s not guaranteed to work, but it’s a first line of defense treatment—a precursor to the more extreme, more expensive, more tedious options. I’d been on the medication before, so reincorporating it into my life was a no-brainer. “Spironolactone inhibits the enzyme that produces testosterone. So it revs that enzyme down, so that you’re not pumping out as much of those hormones,” Dr. Palep explains.

The second treatment, which I decided to do a few months down the line, is something called PRP. Unlike other hair growth treatments like topical minoxidil or Rogaine, this process is chemical-free. It quite literally uses your own bodily fluids to treat your issue. The treatment takes your own blood, spins it in a centrifuge, and injects it back into your scalp—it’s thought to be a very safe process. “We extrapolate your platelets from your growth factors and then reinject it back into your scalp to regrow your hair,” says Dr. Palep. While there aren’t many large-scale studies on PRP for hair growth, most doctors have found via experience that three to four treatments, spaced four weeks apart, work best at the get-go. Once you’re at a good place, bi-yearly maintenance treatments are recommended.
It’s a toss-up—per person—on whether or not the whole process will work. And it doesn’t come cheap. One session can cost upwards of $1,000. In short: It’s risky. I was lucky enough to get three PRP treatments free of cost, thanks to the amazing Dr. Arash Akhavan, founder of The Dermatology & Laser Group. During my first appointment, we went over the basics, took preliminary photos, and discussed the process. My hair loss admittedly is not as far along as other people’s. I’m not going to be the photo that pops up when you google “androgenic alopecia.” My follicles were intact, my part was only ever-so-slightly widening, and I still had a full head of hair. To the naked eye, I was just dandy. My results, Dr. Akhavan said, would be more based on feel.
We were trying to get my texture back. My density. My length. I’d lost over half of my hair—and I wanted it back. “There are specific growth factors that we can isolate that send signals to the hair follicles. There’s vascular endothelial growth factor (VEGF), something called fibroblast growth factor, and platelet derived growth factor,” he explains. “The hair gets a boost of these growth factors from the PRP, so you have more chemicals telling that root to produce thicker, longer, healthier hair.” Existing hair becomes stronger and new hair is better suited to last—and grow.
I’d lost over half of my hair—and I wanted it back.
My blood was drawn (approximately four vials), it was taken into the back where the spinning happens, cooled down, and brought back to my room. I was warned: This would hurt. It’s needles that go straight into the scalp—not pleasant. The good news: I have a freakishly high pain tolerance and Dr. Akhavan is a master of distraction. He used a medical vibrator to detract from the pain. It’s like a mental exercise. Focus on the vibrations, not the needles. The pain, while not unbearable, was short-lived—thank god. It took about two minutes for Dr. Akhavan to inject my own blood into the crown of my head. There’s a little residue, but it got cleaned up, and then I was sent on my way with two Advil to boot. I was sore and I could feel little blood bubbles raised on my scalp where the needles went. Weird, but worth it.
I repeated the PRP process four weeks later. Quite frankly, I didn’t think it was working. I was about to be a part of the percentage that sees little to no difference. Le sigh. “It takes months to see the results,” says Dr. Akhavan. “You need healthy hair to grow out of your scalp and then, especially if your long hair, kind of make its way to some sort of substantial length.”
Then, a few weeks after my last injection, I started to feel like my hair was getting thicker. Maybe I was being delusional or imagining things, but my roots felt denser. Hell, I was even brave enough to go get a haircut, something I hadn’t done in over a year for fear of losing my last little bit of length that I had clung to like my life depended on it.
But fast forward a few weeks yet again, and I entered my third PRP appointment with what I started to call alfalfa sprouts coming out the top of my head. It was new hair growth growing straight up. Cute? No. But part of the process. It was only a matter of time before baby hairs popped out on the upper corners of my head.
Now, I’m six months out from my initial treatment. My length is by no means what it used to be, or what I want it to be. It’ll take time. Hair can only grow half an inch per month. But my hair feels like my hair again. It’s thicker. It’s getting there. I’ll be locked into maintenance treatments for life if I want to maintain my results. Unfortunately, it’s not a three treatments and done situation. I have androgenic alopecia in my 20s. In a couple decades, most of my friends will be dealing with the same form of thinning. It’s a fact.
Interestingly, my hair remains an integral part of my identity. It’s taken up a different form, for sure. But hell, I talk about it more now than I ever did before. What have I learned? Everyone has a hair story, a shedding experience, or a little bit of hormone-induced aesthetic trauma. In the same vein, each person has a tip, trick, or miracle supplement they swear by. Mine, just so happens to be getting my own blood shot into my scalp.

Samantha Holender is the Senior Beauty Editor at Marie Claire, where she reports on the best new launches, dives into the science behind skincare, and shares the breakdown on the latest and greatest trends in the beauty space. She's studied up on every ingredient you'll find on INCI list and is constantly in search of the world's glowiest makeup products. She's constantly tracking the biggest nail and hair trends to pop up in the beauty space, going backstage during fashion weeks, tracking celebrity looks, and constantly talking to celebrity hair stylists, nail artists, and makeup artists. Prior to joining the team, she worked as Us Weekly’s Beauty and Style Editor, where she stayed on the pulse of pop culture and broke down celebrity beauty routines, hair transformations, and red carpet looks. Her words have also appeared on Popsugar, Makeup.com, Skincare.com, Delish.com, and Philadelphia Wedding. Samantha also serves as a board member for the American Society of Magazine Editors (ASME). She first joined the organization in 2018, when she worked as an editorial intern at Food Network Magazine and Pioneer Woman Magazine. Samantha has a degree in Journalism and Mass Communications from The George Washington University’s School of Media and Public Affairs. While at GWU, she was a founding member of the school’s HerCampus chapter and served as its President for four years. When she’s not deep in the beauty closet or swatching eyeshadows, you can find her obsessing over Real Housewives and all things Bravo. Keep up with her on Instagram @samholender.