Let's Decode Your Acne, Shall We?
How to identify—and treat—every shape, size, and type of pimple.


Hello and welcome to your very own acne crash course. Here’s the thing: We’ve all had a pimple, a breakout, heck, even an acne battle to contend with over the years. It’s normal—like so, so, so normal. But, if you are on the hunt for clearer skin, we feel you! We hear you! We got you! The first step? Identify the type of acne you're dealing with. Comedones, a.k.a. whiteheads and blackheads, are going to require a slightly different approach than a deep cystic or nodular pimple. Reason being, you need to address what’s causing you to break out in the first place. Occasionally hormonal fluctuations that coincide with your menstrual cycle are to blame, sometimes it’s congestion, and other times you’ll be dealing with wild inflammation.
But through it all, dermatologists (and our handy-dandy guide to the different types of acne) should be your guiding light. Because whether you’re dealing with flares in your teens or are part of the 22 percent of women that develop adult acne, there are over the counter products (benzoyl peroxide! salicylic acid! adapalene!) and prescriptions that can calm down inflammation, prevent your pores from becoming clogged, and regulate hormones. Here, we’re explaining what each type of pimple looks like, what causes it, and how to treat every type of acne.
Is My Acne Mild, Moderate, or Severe?
We can tell you how to treat every type of acne with skincare products until we’re blue in the face, but over-the-counter skincare products are only half of the equation. While they can do the job for mild and some moderate acne, they’re not going to be enough for someone with severe acne. If you fall into the latter category or can't manage your moderate acne alone, you’ll probably need to pair your OTC cleansers and moisturizers with prescription topicals and oral medication. So, how do you know which group you fall into?
According to Dr. Robert Finney, board-certified dermatologist at Entieré Dermatology, mild acne is categorized by occasional breakouts that last a few days’ time. You might have some lingering hyperpigmentation, but it traditionally fades pretty quickly. “Moderate acne is when you’re starting to get some deeper pimples, they’re coming more regularly, and it’s actually more infrequent that your skin is clear. Once these flares do clear up, you’re left with marks that last for a little while,” he explains. “You’re closer to severe acne if you’re constantly having cystic lesions, you have signs of scarring from your acne past, and the breakouts last for a long time.”
The Types of Acne
“There are five main types of acne lesions,” explains Dr. Shari Marchbein, board-certified dermatologist and founder of Niche Dermatology. “Blackheads and whiteheads are your foundational acne that leads to all other acne. Even small acne can turn into cystic lesions and lead to scarring and pigmentation, so it’s worth treating even the most mild of acne.”
- Blackheads: Resulting from a clogged pore that has oxidized, this non-inflammatory acne presents as a little black dot.
- Whiteheads: Similar to a blackhead, a whitehead happens when a pore gets clogged. The difference is that whiteheads will typically have pus and inflammation.
- Papules: If you have a dense, pus-less red bump on your skin, chances are you're dealing with a papule. Don't try and pop it—you'll get nowhere.
- Pustules: Typically oozy, pus-filled (peep the name), pustules are typically accompanied by tender inflammation and discomfort.
- Cystic-Nodular: You'll most commonly find cysts on the lower third of your face, as they're traditionally hormonal in nature. They're also referred to as "blind pimples," because while you will certain feel their inflammaion and tenderness, they live under the skin.
The treatment, says Dr. Finney, is dependent on which camp your acne falls into: Inflammatory (a.k.a. red and swollen) or non-inflammatory (a.k.a. skin-colored and congested). Inflammatory acne is going to be treated with antibacterial ingredients like benozyl peroxide, as well as oral medication, whereas non-inflammatory acne is best treated with ingredients like salicylic acid. For a more detailed breakdown on each type of acne and the accompanying treatment, keep reading.
What Is a Blackhead?

Marked by a little black dot, blackheads are pretty easy to identify. “These are your congested and clogged open pores,” says Dr. Finney. They form when the opening of your hair follicle gets plugged up with oil, dead skin cells, or a mixture of both. Think: The more oil and more dead skin cells you have, the more likely you are to develop a plug. Then, when that collective gunk touches the air or interacts with pollution, it’s thought to oxidize and turn black.
Get exclusive access to fashion and beauty trends, hot-off-the-press celebrity news, and more.
Blackheads are most likely to pop up on your T-Zone thanks to the high concentration of sebaceous glands (a.k.a. oil glands), but they’re also very common on the chin, back, and chest. It really depends on your skin’s makeup. “Follicles aren’t all created equal in size, toughness, or dexterity,” explains Dr. Finney. Men for instance may be more prone to have ruptured follicles where they shave, while others may have certain areas of follicles, like the on the nose, over-producing oil.
How to Treat a Blackhead
“Treatments targeting congestion and breaking up oil—like your salicylic acids, your Differin gels, and your exfoliants, are really going to help,” says Dr. Finney. That in mind, his first recommendation is typically going to be a retinoid, like over-the-counter adapalene or a prescription formula. While retinoids do have a multitude of benefits (read all about 'em in our comprehensive guide to retinols and retinoids), not everyone can tolerate the drying effects of a retinoid. “If you can’t tolerate a retinoid, my go-to prescription for congestion is azelaic acid. It targets congestion, but it’s also going to block hyperpigmentation.”
You’re also going to want a lightweight, non-comedogenic gel moisturizer to combat the drying effects of the treatment, whether it’s OTC or from the dermatologist. (Reminder: Any time you're using a retinoid or exfoliant, it's even more important to wear a broad-spectrum SPF.)

The original over-the-counter retinoid, Differin gel is one of the best blackhead-busting products. It might take a minute. for your skin to get adjusted to the vitamin A derivative (expect some flaking and dryness for approximately six weeks), but your T-zone will thank you in the end.

Multi-purpose by design, this salicylic acid, azelaic acid, and licorice root extract targets every stage of your pimple. It can prevent clogged pores, while simultaneously addressing the inflammation and redness of current acne legions.
What Is a Whitehead?

Considered a closed comedone, whiteheads are typically going to be red at the base and have a little pus-filled head that is admittedly tempting to pop (don’t do it, people). What causes it to form, you ask? It’s very similar to the formation of a blackhead. The follicle ruptures thanks to the perfect storm of oil, dead skin cells, and bacteria overgrowth. Unlike a blackhead however, there’s an added layer of inflammation to address.
“If there’s still oil production trying to get through once you have a blockage, it builds up behind it,” says Dr. Finney. “Bacterial overgrowth loves that inflammatory environment down there and creates micro-ruptures, the red appearance, and can eventually lead to the whitehead.” While there’s a very obvious blockage (peep the white pus), it’s still superficial in nature and located in the dermis, which is the uppermost layer of the skin. Pustules and cysts (we dive into those in a bit), are going to be rooted much deeper in the skin.
How to Treat a Whitehead
One of the best over-the-counter treatments for whiteheads is going to be benzoyl peroxide, says Dr. Finney. “It’s going to be the strongest as a leave-on,” he explains. “Washes can help, but they’re only short contact. Anything that’s only sitting there for a few minutes is going to have less of an impact than something that you’re leaving on.” He also suggests incorporating either a retinoid or an azelaic acid product into your routine to help with congestion. And of course, use a sunscreen and moisturizer designed for acne-prone skin.
It’s also just as, if not more, important to keep your hands off your acne—no matter how tempting popping can seem. “It’s as if you’re seeing the tip of an iceberg with your whitehead. If you’re pressing on the tip, you’re also putting pressure on what’s going on underneath the surface. You can cause that follicle that’s already ruptured to rupture even more and bring more inflammatory cells,” Dr. Finney explains. “That’s why sometimes when you pop a pimple, it can turn into a whitehead again—and with more inflammation.” If you don’t trust yourself to keep your hands off, use a pimple patch. Dr. Finney recommends one with a hydrocolloid dressing, a little bit of salicylic acid, and micro-darts, all of which can “coax the gunk to come out.”

Another La Roche Posay gem, Effaclar Duo is a great overnight spot treatment for a pesky whitehead. Pop a pea-sized amount on any affected area and prepare for inflammation and irritation to dissipate.

Popping a clear pimple patch, such as this one, on top of a whitehead is not only an effective method for forcing the white head out, but it also prevents your fingers from adding additional bacteria into the mix.
What Is a Papule?

Baseline: “A papule is a raised bump on the skin’s surface that is less than one centimeter in size,” says Dr. Robyn Gmyrek, board-certified dermatologist at UnionDerm. “They usually develop from excess oil and dead skin cells clogging a pore.” Unlike a blackhead or whitehead though, papules are going to be solid, have no pus, and can be either red, flesh colored, or brown. While it’s not necessarily a prerequisite, Dr. Gmyrek explains that they can be tender if inflammation is involved. Anyone can get a papule, but they’re most common among oily skin types. Sensing the theme where oil is the culprit?
A quick caveat: Papules aren’t always acneic in nature. They can also pop up after shaving. “A papule arises after shaving when the hair is trying to grow above the surface but meets resistance by dead skin cells clogging the follicle. The hair might then grow into the skin instead of out of the follicle,” explains Dr. Gmyrek. In response, the body triggers an inflammatory response to push the hair out. Enter: A razor bump. The same can be said for the papules that form after a bug bite or sting. That in mind, these two incidences are not acneic in nature and need to be treated differently.
How to Treat a Papule
When treating a papule, you’re going to want to focus on decreasing bacteria, inflammation, and oil production. The best-antibacterial ingredient is going to be benzoyl peroxide. If your acne is more moderate or severe, your dermatologist may put you on prescription clindamycin lotion or pads. If your papules have inflammation, Dr. Gmyrek suggests over-the-counter adapalene or niacinamide, a gentler option. And for oil buildup? Salicylic acid, azelaic acid, and retinol are considered effective ingredients.
Just to reiterate: Don’t overdo it with active ingredients. Start with one product at a time to see how much your skin can handle. When in doubt, or if your acne is more severe or bothersome, go to the dermatologist. They might recommend prescription topicals, like Aczone, suggest Accutane, or put you on hormone blocking medication such as birth control or Spironolactone if your breakouts are correlated to your cycle.

Because this type of pimple is inflammatory in nature, finding a cleanser that's antibacterial in nature is ideal. And this CeraVe option has an unbeatable price point. It works up into a nice foam and leaves skin feeling clean—not stripped.

Niacinamide is a powerhouse ingredient with benefits that could be listed a mile long. Any serum that features the multi-purpose will do, but this Ordinary one is great if you're shopping on a budget. The concentration is ideal for reaping the soothing benefits sans irritation.

In case you haven't received the memo yet, retinol and acne are a dream team. While drugstore options will do the job, this SkinCeuticals night treatment is particularly ideal for first-timers. The concentration is a starter dose, so your skin can really get acclimated to the powerful ingredient.

Per Dr. Gmyrek, azelaic acid is a great ingredient to incorporate into your acne-fighting skincare routine—especially if your skin is on the oily (and sensitive) side. Moisturizing and soothing ingredients have also made their way into this formula, making it ideal for blemish-prone, but easily irritated skin.
What Is a Pustule?

“A pustule is defined as a papule that is not solid, but rather filled with white or yellow pus,” explains Dr. Gmyrek. “They start the same as a papule, but the body responds with a greater immune response that causes more inflammation, so there may be a greater bacterial load, too.” Think of a pustule like the papule's angrier big sister. “Pus is a natural result of the body fighting infection. It is a thick white or yellow fluid made up of dead white blood cells that the body has sent to kill infection, dead skin cells, and residual bacteria.”
While pustules can be nipped in the bud (read below), it is possible for them to escalate into a more severe form of acne. “If a pustule is very deep on the skin or if your body’s immune response is not strong enough to kill the infection, the pustule can become a deep nodule requiring antibiotic treatment,” adds Dr. Gmyrek.
How to Treat a Pustule
“When a patient presents to me with pustular acne, I know that they have excess oil and clogging of their pores, which has led to acne. They have a strong inflammatory response by their immune system and they have bacteria contributing to this process so, I try to address all of these components,” explains Dr. Gmyrek. As such, she treats pustular acne the same way as papular acne with products that are antibacterial (benzoyl peroxide), anti-inflammatory (niacinamide or adapalene), and de-clogging (salicylic acid, azelaic acid, retinoids).
Because pustules come along with more inflammation, they can be uncomfortable and can be more prone to scarring, so you may be more likely to seek treatment with a board-certified dermatologist. They will likely put you on a regimen that address all three causes with prescription retinoids, topicals, oral antibiotics, or hormonal therapy to control oil production.

Surprise, surprise: You want a retinol to treat your pustules too. If you're not going to go the prescription route, I cannot recommend Shani Darden's formulation enough. It's truly the perfect blend of hydrating ingredients and exfoliating actives. Give it a true six weeks to work its skin clarifying magic.
What Is a Cyst?
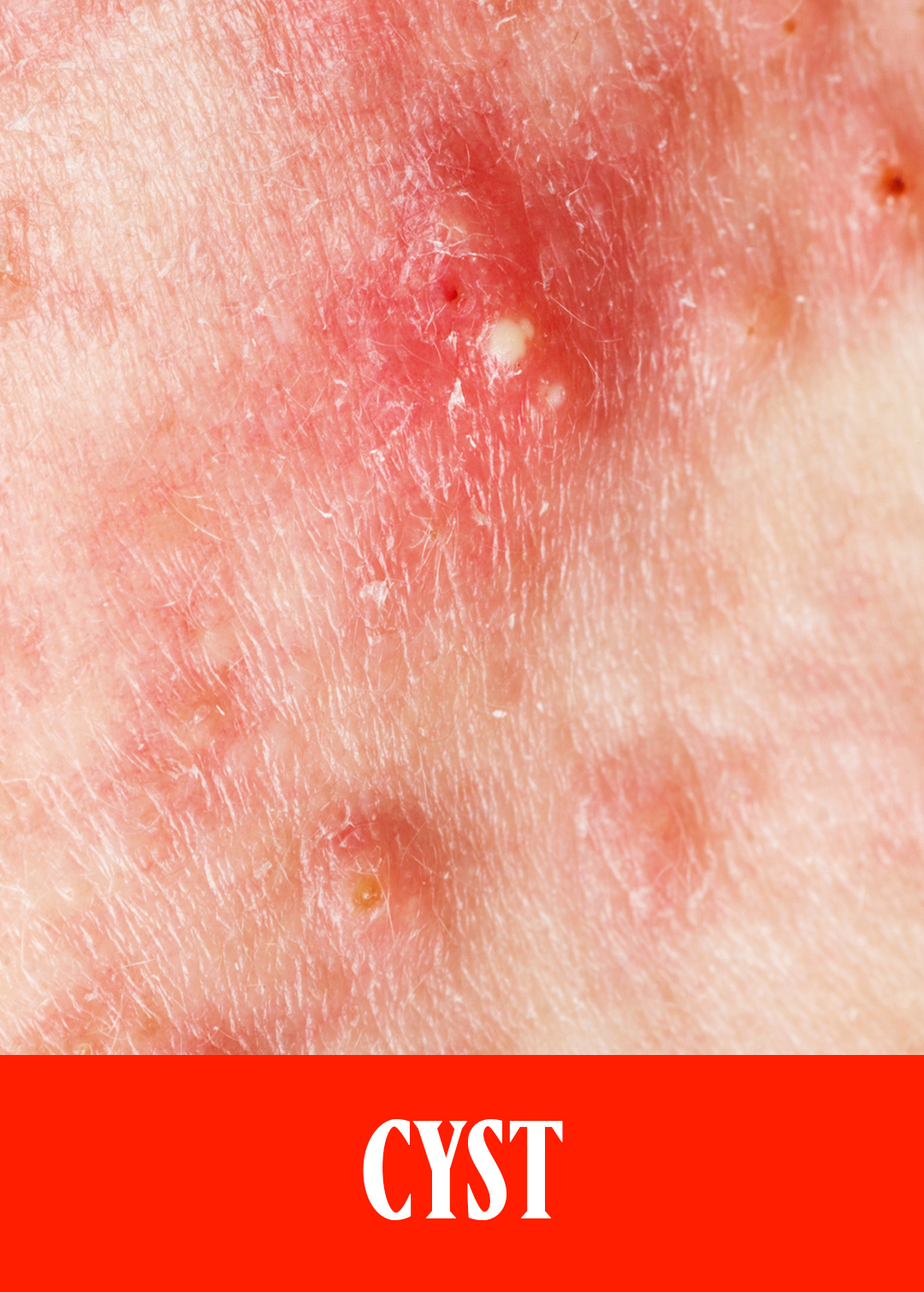
“Cysts are the largest, most painful form of acne lesions,” explains Dr. Marchbein. “They tend to be almost underground, become more inflamed, and are more painful. They’re also the ones that tend to lead to more scarring and hyperpigmentation.” Cysts can pop up anywhere and at any time, but it’s worth noting that they’re commonly hormonal in nature and very common in adult female acne. “They tend to be on the lower third of the face and upper neck.”
If you have larger cysts, or multiple cysts that form in close proximity to one another, you might fall into the nodulo-cystic category of acne. “Nodules are a form of large cysts—they’re synonymous.”
How to Treat a Cyst
This type of acne almost always requires “more aggressive treatment,” according to Dr. Marchbein. While topicals like benzoyl peroxide, retinoids, and prescriptions like dapsone can help treat the “stickiness” of the cells, speed up cell turnovers, and address other types of acne that occur in tandem with cysts, nodulo-cystic lesions usually require oral medication. “For females, birth control and Spironolactone are our mainstay for treating cystic lesions,” explains Dr. Marchbein, noting both help regulate hormones. Your doctor may also prescribe oral antibiotics for a short period of time. “When someone has cystic lesions that are large, painful, and actively scarring, that’s an emergency for us—scarring is permanent. We’ll often combine treatments with oral antibiotics to put out the fire as quickly as possible.”
Another medication that your doctor may suggest is something called Accutane, which is considered the closest thing to a “cure” for acne. “Accutane, which is an oral form of vitamin-A, is FDA-approved for cystic, scarring acne, or acne that’s unresponsive to other treatments,” Dr. Marchbein explains. It can have drying side effects, cannot be taken if you’re trying to get pregnant (you need to be using two forms of contraceptives), and the treatment needs to be closely monitored by a dermatologist. While it is a great option, Dr. Marchbein explains that adult female acne is better treated with hormone-regulating medications.
The last noteworthy treatment for cystic acne is a cortisone shot. “We call it a cortisone shot, but it’s really a steroid called kenalog. We dilute it so it’s a very low, low, low dose version and then we inject it superficially into the pimple to help bring down redness, pain, and inflammation,” says Dr. Marchbein. “Doing this will also help reduce the potential for scars and pigmentation.” You want to jump on this as quickly as possible, so call your dermatologist as soon as you notice tenderness and swelling. Cortisone shots are perfectly safe, however it’s important to make sure you’re seeing a well-trained provider. If the injection is placed too deep or used on too small of an acne lesion, it can “atrophy” the skin and leave you with an indentation.
For more information on acne, check out our stories on the best acne spot treatments, hormonal acne, and the best sunscreens for acne.
Meet the Experts

Originally from Pittsburgh, PA, Dr. Finney completed his undergraduate and medical degrees at Pennsylvania State University. He completed his internship and dermatology residency at Thomas Jefferson University Hospital in Philadelphia, PA where he served as chief resident during his final year. He also performed a postdoctoral research fellowship in eczema and allergic contact dermatitis at Rockefeller University in addition to an advanced fellowship in aesthetics, hair restoration, and skin surgery with renowned hair surgeon Dr. Marc Avram in New York. Dr. Finney is a clinical assistant professor at New York University Langone and teaches future dermatologists at Bellevue Hospital.
Dr. Finney is an expert in medical, surgical, and cosmetic dermatology and is regularly asked to contribute to various media outlets, including Men’s Health, Men’s Journal, Esquire, and Women’s Health. He does not approach aesthetics from a cookie-cutter approach, rather he works closely with each patient to design a customized treatment regimen to achieve his or her desired aesthetic outcomes that appear natural and refreshed, never over-done.

Dr. Shari Marchbein is a board-certified dermatologist and a fellow of the American Academy of Dermatology. Dr. Marchbein’s academic and clinical interests include the treatment of acne, in particular adult female acne, acne scarring, and rosacea. She also specializes in various aesthetic procedures and laser surgery. Dr. Marchbein has been sought out as a leader in her field for the treatment of acne and rosacea and has published multiple articles on acne pathogenesis and treatment.
She has presented at renowned national conferences on the topics of acne and rosacea, including the annual American Academy of Dermatology and Advances in Dermatology meetings. Dr. Marchbein earned her Bachelor of Science degree from the State University of New York at Binghamton where she graduated Summa Cum Laude and became a member of the Golden Key National Honor Society and Phi Beta Kappa National Honor Society.
Robyn Gmyrek, M.D. is a Board Certified dermatologist that has received national recognition for her contributions to cosmetic dermatology, including Castle and Connolly America’s Top Doctors, New York Magazine’s 2013-2020 Best Doctors, and inclusion in the 2013-2020 lists of Super Doctors. Before joining UnionDerm Dr. Gmyrek was on the faculty of Columbia University Medical Center where she was Division Chief of Cosmetic Dermatology and founded Columbia University’s Cosmetic Skin and Laser Center. At Columbia, Dr. Gmyrek also was the Director of the Resident Cosmetic Clinic, instructing the resident physicians in cosmetic procedures, and was in charge of the Fourth Year Medical Student Electives in Dermatology.
Dr. Gmyrek received her Bachelor’s degree from New York University where she graduated Phi Beta Kappa and Magna Cum Laude. She went on to complete her medical school education at Columbia University, College of Physicians and Surgeons. After graduation, she finished an internal medicine internship at Cornell University – New York Hospital. Dr Gmyrek then returned to Columbia’s College of Physicians and Surgeons where she completed her dermatology residency training, served as Chief Resident in Dermatology, and in 2000 joined the full time faculty of the Department of Dermatology.

Samantha Holender is the Senior Beauty Editor at Marie Claire, where she reports on the best new launches, dives into the science behind skincare, and shares the breakdown on the latest and greatest trends in the beauty space. She's studied up on every ingredient you'll find on INCI list and is constantly in search of the world's glowiest makeup products. She's constantly tracking the biggest nail and hair trends to pop up in the beauty space, going backstage during fashion weeks, tracking celebrity looks, and constantly talking to celebrity hair stylists, nail artists, and makeup artists. Prior to joining the team, she worked as Us Weekly’s Beauty and Style Editor, where she stayed on the pulse of pop culture and broke down celebrity beauty routines, hair transformations, and red carpet looks. Her words have also appeared on Popsugar, Makeup.com, Skincare.com, Delish.com, and Philadelphia Wedding. Samantha also serves as a board member for the American Society of Magazine Editors (ASME). She first joined the organization in 2018, when she worked as an editorial intern at Food Network Magazine and Pioneer Woman Magazine. Samantha has a degree in Journalism and Mass Communications from The George Washington University’s School of Media and Public Affairs. While at GWU, she was a founding member of the school’s HerCampus chapter and served as its President for four years. When she’s not deep in the beauty closet or swatching eyeshadows, you can find her obsessing over Real Housewives and all things Bravo. Keep up with her on Instagram @samholender.






